Understanding ME and Chronic Fatigue Syndrome in Children

Longterm and little-understood illnesses like ME, or chronic fatigue syndrome, can leave pupils misdiagnosed, isolated and forgotten, so it pays to spot the signs, says Claire Tripp…
- by Claire Tripp
You leave work with “Miss! Miss!” still echoing in your ears, an armful of marking, and thinking of Ellie.
Once bright-eyed and eager to learn, today you spotted her nodding off in the corner.
You know it definitely couldn’t have been your lesson on coordinating conjunctions, so make a mental note to speak to her again tomorrow to check she’s OK.
But Ellie doesn’t make it into school tomorrow because her mum says she’s not well. In fact, Ellie hasn’t been to school regularly since she was in Y4.
The medical evidence says she has chronic fatigue syndrome (CFS). School thinks this means she’s just exhausted and can’t cope with everyday life.
Instead, she’s seriously ill and coping with more than they could imagine.
Long haul
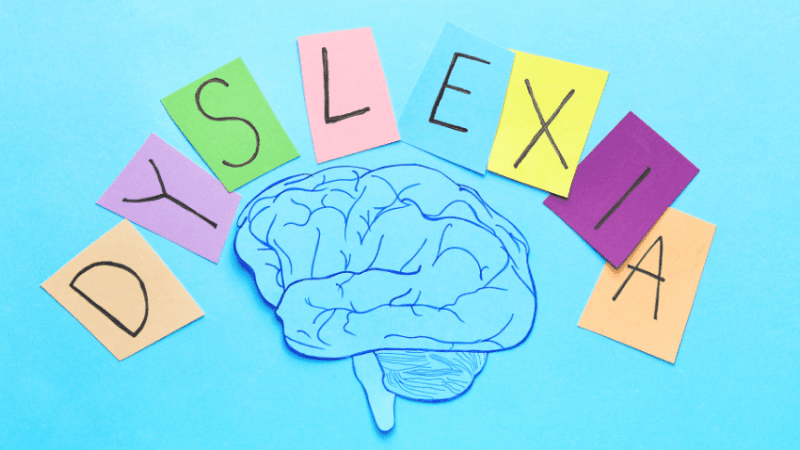
An estimated 1% of school-aged children suffer from CFS, more widely known as ME (myalgic encephalomyelitis).
Although more well-known in teenagers, ME can actually affect children from as young as five. It’s the most common cause of longterm sickness absence from school and studies show that 68% of children need an average of five years to recover and get their lives back on track.
(Those outside of that statistic need longer or don’t recover.) A devastating prognosis for a young child.
Yet their absence is typically treated by schools as an attendance problem.
This means primary pupils don’t receive the kind of pastoral care we should be giving a child with a serious illness and, more often than is acceptable, it can lead to unjustified and traumatic safeguarding proceedings for the family.
It’s hard to appreciate just how debilitating ME is. Most symptoms are invisible: cognitive dysfunction affects a child’s ability to learn, severe muscle pain gets worse after light activity.
People with ME suffer from extreme exhaustion, but young children can often become hyped up from overexertion temporarily masking symptoms.
Ellie’s life isn’t spontaneous any more. Every drop of energy is valuable and daily activities are limited and carefully balanced so that, instead of just existing, she has some semblance of living.
She’s finding it really tough to be ill for so long. She’s disabled, not tired. And she’s certainly not ‘avoiding school’.
It’s easy to underestimate the physical and mental demands of being at school. Children with ME report going to school is the single most energy-draining thing they can do.
Yet it’s the activity they find the most distressing to be missing out on and are most determined to resume.
The risk of being forgotten by their classmates and teachers is high. Life moves fast in primary school.
Children with ME spend large parts of their childhood socially isolated, and in many cases struggle to access an education.
It’s a lonely existence when their friends are falling in and out of friendship groups or still laughing about when Miss accidentally set the fire alarm off.
Spotting the signs
The good news is that early identification and the right support for a child with ME suggests they have a greater chance of recovery than adults.
This is where schools play an important role. But when young children are known to put on a brave face and pretend everything’s OK, how are we supposed to know what’s really going on?
Particularly when, due to an historic lack of medical education on ME, even doctors can find that difficult?
Fortunately, ME has a unique symptom called post-exertional malaise (PEM), which means symptoms worsen or increase even after the smallest amount of activity.
This can be seen if a pupil has to go home early on a regular basis or is struggling to concentrate towards the end of the school day.
So spotting patterns can be a sign that something is wrong.
Trending
The full picture
While many children may be able to come into school for a full day, they can collapse into bed as soon as they get home.
So schools need to work with parents to build up an overall picture of health and should recognise that they only get a snapshot of a pupil’s day.
ME fluctuates from day-to-day and is hard to predict. So healthcare plans and timetables have to be highly flexible with the child’s health and education goals in mind, not attendance.
Whether we think school should be at the top of the list or not, it’s only one piece of the puzzle when looking at the future.
So, a healthy balance of education, socialisation and development is needed.
Pupils with long-term illnesses should feel part of the school, even if they aren’t well enough to be there.
They should be encouraged to come into school for the fun activities too, not just for maths and English.
No one expects school staff to fully understand ME; it’s a highly complex illness and poorly understood by even the medical profession.
The key is to seek advice from experts, who can take a pragmatic, informed approach in helping schools, children and families with managing education, safeguarding requirements and a child’s health needs.
Tymes Trust, for example, is an ME charity for young people run by a former headteacher and directly helps and advises schools and SENCOs with pupils who have ME.
See more at tymestrust.org.
Members of staff need time and patience to listen and learn about the child’s condition and what support they need.
It’s important that schools recognise how ME could be a cause for regular absence or loss of engagement in class. Families should be spared unnecessary accusations and suspicion.
Despite what they might say to the contrary, most children would be devastated if forced to miss such a huge chunk of school.
Those who do miss out deserve care and compassion, understanding and support. Just as we would give any other child with a long-term illness.
ME – the lowdown
An ME diagnosis can be difficult to get due to lack of medical awareness and can take months. If ME is suspected, support should be put in place straightaway to protect the pupil from further deterioration.
- Physical and mental symptoms should not be ignored or minimised, or motivation confused with energy levels. Children should be believed when consistently reporting pain or cognitive dysfunction after activity as this is a key symptom of ME, which is not always visible.
Claire Tripp manages her daughter’s SEN education and campaigns for health equality with #MEAction. Follow her on Twitter at @chicaguapa.